Healthy Internal Boundaries
Apr 29, 2021
How your gut health determines your immune capacity
Digestive health is crucial to all body functions; to provide what they need and keep out potentially harmful cells and tissues. The gastro-intestinal tract (gut) is responsible for digestion, absorption and assimilation of nutrients and elimination of waste and toxins, but less known is its role in immunity – not just within the gut, but throughout our whole bodies.
Just like the skin on the outside of our bodies, the gut wall is essentially a barrier, constantly decided what is safe to allow inside and what should be kept out. Until food is absorbed into the body and remains in the gut, it is essentially outside the body – like that piece of undigested sweetcorn in the toilet bowl! Health of the gut wall (gut mucosa) is crucial for integrity of our defences and is sensitive to our emotional, stress and trauma responses.
The gut-immune-stress connection
The main anti-inflammatory part of our immune system is housed in the mucous linings of the digestive, respiratory and urinary tracts. These link directly to the lymphatic system; the route by which lymphatic fluid delivers foreign and toxic agents to these sites where they are killed and destroyed. This protection at these barriers particularly at the gut and lungs is as an important part of our innate immunity; our first line generalised immune defences of which inflammation is also a key part. Yes, we need specific (acquired) immunity developed against specific invaders (such as COVID-19 or influenza) but our ability to fight these off and how severe (or even fatal) these can be, are very much dependent on the health of the linings (epithelia) of these internal passageways.
It is the beneficial bacterial colonisation – microbiome, probiotics or ‘good gut flora’ – at the gut and lungs that not only determine the quality of our immune responses, but we are also understanding how this also reaches out into our mood, energy, appetite and more. In the gut, a healthy microbiome can contain 7lb of beneficial or ‘probiotic’ bacteria; heavier than of all of your skin cells. These good bacteria are altered or lowered by stress, sugar, alcohol, antibiotics and pharmaceutical medications (Alcohol Res. 2015;37(2):223-36/ Obes Rev. 2012;13(9):799-809/ Neurobiol Stress. 2017;7: 124–136/ Trends Mol Med. 2016;22(6): 458–478/ Br J Pharmacol. 2018 Dec) in ways that may contribute to irritable bowel syndrome (World Journal of Gastroenterology. 2014;21; 20(39)14105), anxiety and depression (Neurotherapeutics. 2018;15(1):36–59).
Immunity on the gut wall is regulated by secretory antibodies (sIgA), low levels of which can result in poor signalling from the gut that result in inappropriate immune responses (like reacting to ‘self’ in auto-immune diseases) or overreaction contributing to inflammatory conditions (eczema, asthma, hayfever, migraines, arthritis, psoriasis). The gut-lung axis describes the constant communication via the gut microbiome and that throughout the respiratory system, with recent research recognising the link between lowered healthy gut bacteria and the lungs; “gut dysbacteriosis might result in chronic inflammatory respiratory disorders, particularly asthma” (Int J Mol Sci. 2019 Jan; 20(1): 123).
Continual and chronic stress has shown to reduce levels of probiotic bacteria and sIgA, tending us to an inflammatory cytokine response (Horm Behav. 2017;88():70-78). Cytokines are immune messengers that raise the alert as the inflammatory cascade begins and can give us flu-like symptoms; they have come to public consciousness recently in relation to the ‘cytokine storms’ or sudden, excessive inflammation seen in more severe cases and deaths.
According to Robert Burk, M.D., professor of paediatrics, of microbiology and immunology, and of epidemiology and population health at the Albert Einstein College of Medicine in New York; “We know from many studies that the gut microbiome has important immunological functions. The microbiome could be contributing to the immune system’s overreaction to the virus—the so-called cytokine storm that overwhelms the lungs and is the main cause of death in patients with COVID-19.” (source)
Dr. Burk has stated that analyses of the gut microbiome before and after people’s coronavirus exposure could help predict which patients with the infection are likely to experience a cytokine storm, and lead to strategies to prevent it from happening. This is an interesting direction, given the findings of a recent study that discussed the evidence that aging alone alters the gut microbiome and likely contributes to age‐related inflammation a condition often referred to as “inflammaging.” The authors concluded that the microbiome can be modified to positively impact outcomes from age‐related diseases, which of course now could include higher age-related vulnerability to COVID-19. (Ann Neurol 2018;83:23–36)
Nutritional support for gut health
As well as some conscious attention to reducing the dietary factors that negatively affect the microbiome – stimulants, refined sugars, alcohol – some key ingredients in your diet can support an immune-healthy gut environment:
Garlic
Garlic acts as a potent prebiotic – meaning it feeds probiotic bacteria – in particular, in research it has shown to stimulate the growth of one of our major probiotic colonisers, Bifidobacterium species (Food Science and Human Wellness,2013;2(3-4):119-123). Garlic has long been used traditionally to as an antimicrobial, reducing and inhibiting the growth of some pathogens (harmful agents) in the gut; its oil has shown to have these properties in research (Journal of Food Protection, 2004;67:499-504) along with its cousins in the allium family, onions and leeks.
Prebiotics
You’ll get loads of these probiotic fuel increasing your vegetable intake, but the highest levels of the prebiotic inulin are found in Jerusalem artichokes, chicory, bananas, garlic, onions, leeks and dandelion leaves (for weeding gardeners out there). Prebiotics have also been shown to help reduce the negative effects of a diet previously too low in omega 3 oils – which may have affected gut-healing abilities. Those on low FODMAP diets may be reducing specific plant foods in the short-term for digestive symptom relief, but supporting the gut environment may allow them to include these beneficial foods longer-term.
Sulphur foods
Daily cruciferous vegetables like cabbage, kale, broccoli and pak choi contain sulphur-based substances called glucosinolates that exhibit powerful biological functions in fighting cancers, cardiovascular and neurodegenerative. Their soluble fibre and nutrient content supports the gut environment, which transforms the glucosinolates into their potent immune-supportive form (J Nutr Biochem. 2019;63:27-34/ J Sci Food Agric. 2018;98(4):1255-1260). They also have anti-inflammatory action within the gut (Nutrition. 2012;28(3):324-30).
Butyric acid
Gut wall cells can be fed by short-chain fatty acids (SCFAs; types of fats) in organic butter (eg butyric acid) and coconut oil (eg caprylic acid), which also support the immune system and metabolic function as antimicrobial agents. Regarded as mediators in the communication between the intestinal microbiome and the immune system (Acta Biochim Pol. 2019;66(1):1-12), SCFAs play a key role in immune modulation and are also produced on the gut wall by the fermentation of dietary fibre. Their presence has also been shown to help reduce the inflammatory effects of chronic psychosocial stress (J Physiol.2018;596(20):4923-4944).
Soups and stews
Add all of the ingredients above and you have a gut-nourishing stew or curry that delivers nutrients in an easily absorbable form directly to the gut cells for nourishment. Cooking long and slow (in a slow cooker or crockpot) replicates how humans have been cooking for nearly 300,000 years (Eur J Clin Nutr. 2002;56 Suppl 1:S42-52); outsourcing energy to break down (digest) food to the heat of fire, rather than using up our own. Cooking long-slow with garlic and onions has also shown to break down potentially inflammatory plant compounds such as lectins and phytic acid and create less gas and bloating; cultures have been doing this the world over since more grains and beans entered our diets in the agriculture ages about 10,000 years ago.
How we eat
How we eat can have as also as much as an impact on gut health as the food itself. Thoroughly chewed food has the best chance of complete digestion and less chance of bringing harmful agents into the body. Our saliva contains a huge amount of immune components; a first line of immune defence that we can miss if quickly gulping down food.
If you have eating habits that tend to the ‘little and often’, this may be putting a strain on your digestive health. This grazing way of eating may support energy levels in the short-term, but continually putting food into our mouths sets us up to become fixated on eating constantly and confuses our relationship with hunger. Eating a fuller meal with the requisite protein and healthy fats creates a sense of satisfaction from the gut to the brain (via neuropeptide messengers in the stomach) that can create a whole-body calming effect; we can relax from the primal imperative to need to seek out more food, at least for a while.
Our digestive tract needs periods where each section of the digestive tract can rest and heal. Constantly having to digest food as we start the process from the beginning again also demands an awful lot of energy. Avoiding snacking between meals wherever possible; it takes up to 40 hours for food to travel from swallowing to out the other end and each time we put something else into our mouths, we start up the whole thing over again and allow little rest for healing.
This isn’t just important to absorb nutrients from our food, but also to ensure that only partially digested food isn’t hanging around, when it can putrefy and create gas and bloating. This debris at the gut wall prevents full digestion and immune function and can lead to symptoms like constipation, diarrhoea and food intolerances.
Mindful eating during meals has shown to naturally regulate portion size and create the satisfaction that lowers food cravings later. Chewing also stimulates the thymus gland to produce T-cells, a major part of the protective immune system; your body knows that unwelcome guests like harmful bacteria may be on their way.
Rest and renewal
Allowing full rest regularly and good quality sleep allows the energy that the gut needs to constantly repair. Thinking, moving and even just standing directs fuel, circulation and nutrients to our muscles and brain. When you consider that the most recent approximation of gut surface marks it the size of half a badminton court and each cell is renewed every 4-5 days, it’s easy to see how our digestive health can suffer without adequate rest. Sleep disruption has shown to alter the gut microbiome and increase inflammatory tendencies and metabolic disruption (Sci Rep. 2016; 6: 35405).
Visceral tissue health – our need to move
When functioning optimally, viscera (organs) has space between organs for ease of movement. Visceral mobility is the ability of organs to rub against and move alongside other organs and tissues. Adhesions that stick tissues of the viscera together can cause obstructions in the fascia (connective tissue), eg portions of the bowel fused together or to other organs; any part of the digestive tract stuck to the wall of the abdominal cavity. We might feel these as internal ‘pulls’ or related to reproductive, pelvic, diaphragmatic or lower back issues as connective tissue in the fascia relates all of the areas as a continual web. An osteopath who works viscerally (as well as structurally) can help feel and ease where such tensions originate and effect.
Visceral motility is the movement that happens within organs eg peristalsis within the digestive tract and can also be affected by mobility issues. Efficient visceral motility allows ease and regulation of bowel movements and supports immune modulation via the microbiome.
Movement for gut mobility and motility
We need to be moving often to provide the fascial ‘slide-and-glide’ that also supports gut motility as well as full physical mobility and reduces fascial lesions that interfere with full digestion. We need to keep hydrated and pliable in the mid-torso area which can become stuck and rigid as we grow older and may even gain weight there. Movement systems such as yoga, dance, belly-dancing, t’ai chi and qi gong where there are differing patterns, fluid motions through the abdominal area and an emphasis on freeing up diaphragmatic movement and breath.
Getting out into nature and having contact with a biodiverse environment as we evolved, is an important component of gut health often missing from those living in urban areas (Proc Natl Acad Sci U S A. 2012;109(21): 8334–8339). Taking our movement patterns and exercise into the countryside is beneficial on so many levels; we humans need wonder and beauty to access the nervous system mode (ventral vagus) that allows gut healing, digestive support through stress reduction and bringing down inflammatory tendencies (Brain Behav Immun. 2018;73: 441–449).
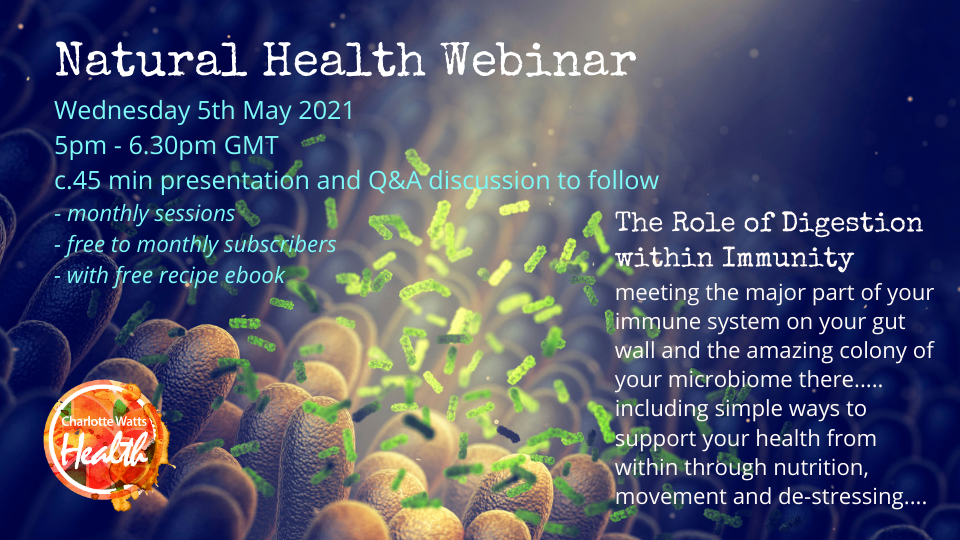
Join Charlotte for her monthly Natural Health Webinars
Next webinar: Wednesday 5th May 2021, 5pm BST
The Role of Digestion within Immunity –meeting the major part of your immune system on your gut wall and the amazing colony of your microbiome there... including simple ways to support your health from within through nutrition, movement and de-stressing - further information here.
Recording available afterwards for monthly subscribers.